- Written:
- Author: Edward
- Posted in: News
- Tags: ciprofloxacin, mitochondria, quinolones
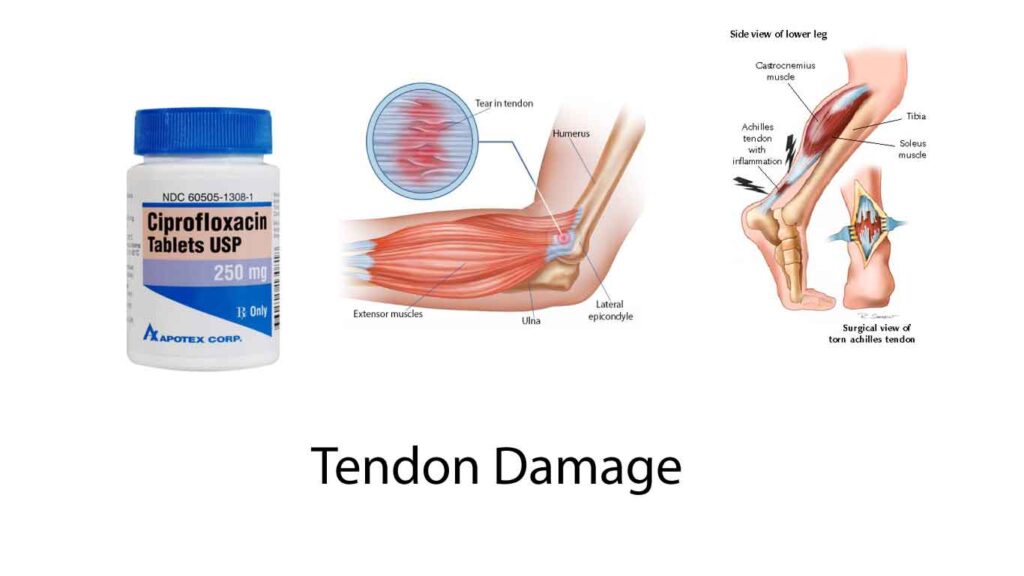
Last week we discussed that doctors have a religious preference when it comes to interpreting Covid-related conditions. This week, I want to share a case of another controversial topic- tendon damage after quinolone antibiotic usage.
LS is a 24 year old man who at the age of 15 received 10 days of ciprofloxacin for prostatitis
A year later, he noticed bilateral patellar tendon pain with exercise. Tendon problems appeared in his hands and then shoulders in the next two years. He received another 10 day course of Cipro at age 18. Tendon problems appeared three years later with the elbows. He received two mRNA shots in 2021 and then the Achilles’, fingers, biceps, and jaw also began to ache. He has been dependent on an immune disrupter to control the pain all over his body.
Believers versus non-believers
If you ask most orthopedic or rehab doctors, they will rarely use quinolone antibiotics; urologists love them on the other hand.
Why the difference? The weight of the denominator tells urologists that since they rarely hear about problems, the drug class is benign. Whereas over the course of a career, the doctors who see the injuries from quinolone use are convinced that a serious rare complication is a good enough reason to avoid this class of antibiotics.
What's the mechanism?
Although there is some controversy, the mechanism appears to be killing of vital energy producing mitochondria in the metabolically active tendon cells. Because these drugs attack the DNA winding enzymes of gyrase and topoisomerase, they are like chemotherapy and inhibit DNA replication. Because they preferentially attack bacteria over human enzymes, they are effective killers of bacteria. Unfortunately, our mitochondria are like bacteria that became symbiotic billions of years ago and they are therefore sometimes vulnerable.
At the ISEV (exosome conference) I recall a lecture where a researcher showed damaged tendons excrete mitochondria-containing exosomes to share energy amidst homeostasis and repair.
It is possible that the patient’s mitochondria were especially susceptible to the effects of the mitochondrial death and it is also possible that he has some stem cell depletion, collagen synthesis disorder, and occult autoimmune disorder targeting the tendon cells and/or the collagen matrices
Can exosomes help?
In general, we have pretty good results with tendon recovery after exosome use. I would say about 60% improve. Keep in mind that if a tendon has tendinosis, this is very different from acute inflammation. The tendinosis makes the structure susceptible to further atrophy and rupture, especially if given corticosteroids. Despite this, doctors often given them, wanting to do something to mitigate pain and risking further atrophy in the process.
In the case of this patient, my prognosis would be guarded. Unlike a normal patient without muscle/tendon stem cell damage and mitochondrial depletion, his existing stem cells may not have the replicative capacity to rebuild through replication.
In the case of a recent consultation with a patient suffering from life-long Duchenne’s muscular dystropy, the prognosis is even more guarded. Although his stem cells have one good copy of the needed gene, many of those stem cells may have undergone loss of heterozygosity (meaning the one good copy is now non-functional), suggesting that the response to the stem cell exosome’s trigger to copy and dedifferentiate might not work as well.
On the other hand, if the ongoing use of immune disruptors is helping his ongoing damage, then an immune suppressive course of exosomes may help to ease symptoms and lead to weaning of the biologic immune disruptors.
We never know until we try.

